Multiple Sclerosis
Category
Autoimmune, Neurological
REVIEWED BY
Our Biomedical Scientist
Reviewed based on
Literature discussion & Clinical Trials
Last update
November 2020
What is Multiple Sclerosis
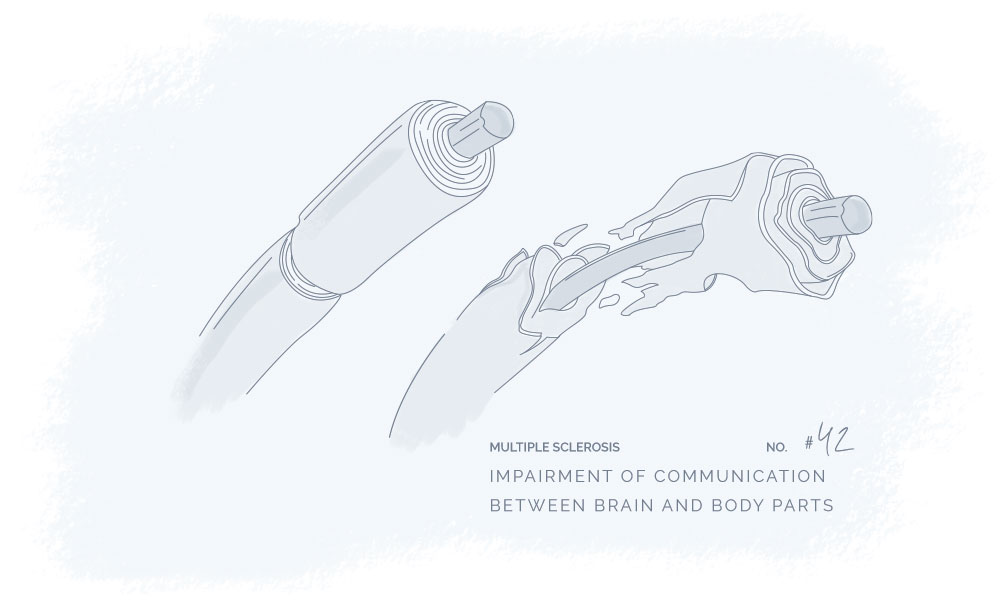
Multiple Sclerosis (MS) is an autoimmune central nervous system disease that affects the brain and spinal cord. In MS, the immune system attacks myelin that covers nerve fibers and leads to problems associated with communication between your brain and other parts of the body.1
Symptoms
Currently, there is no cure available to treat MS. However, treatments can provide modification of the disease course, manage symptoms, and improve recovery from attacks.
Many people suffering from MS have a relapsing-remitting disease course that involves periods of new symptoms or relapses that develop over a period of time and ameliorate partially or completely.
Signs and symptoms of MS can vary between people.1
Most symptoms are related to movement and vision and may include the following:
Movement symptoms
- Weakness or numbness in one or more limbs
- Electric-shock sensations that occur with certain movements
- Tremor
- Lack of coordination
- Unsteady walking pace
- Spasms
- Muscle stiffness
Vision symptoms
- Partial or complete loss of vision often accompanied by painful eye movement
- Double vision
- Blurry vision
Other symptoms
- Slurred speech
- Fatigue
- Pain and/or stinging in part of the body
- Difficulty with bladder, bowel, or sexual function
Cause
Multiple sclerosis is believed to be an autoimmune disease even though the exact cause of its development is not yet known. This malfunction in the immune system leads to the fatty substance destruction that coats and insulates nerve fibers in the brain and spinal cord.1
Factors that can increase the risk of MS are:
- Age
Commonly occurring in the age of 20-40 years old, however, all ages can be affected - Sex
Women are 2-3 times more likely to develop MS than men to have relapsing-remitting MS - Heredity
Genetics may increase the risk of developing MS - Infections
Particular infections including Epstein-Barr may be linked to MS - Race
White people, especially of Northern European heritage have the highest risk of developing MS - Climate
MS are overrepresented in countries with a temperate climate - Smoking
Smokers are more likely than nonsmokers to develop a second event that confirms relapsing-remitting MS
The connection between Cannabinoids & multiple sclerosis
Studies find that CBD and THC may have great therapeutic potential and may be used to help treat Multiple Sclerosis. CBD and THC are well-known cannabinoids, however, they do not have the same psychoactive effects. THC is psychoactive while CBD does not possess psychoactive effects. According to WHO guidelines, the cannabidiol CBD is generally well tolerated with a good safety profile.
Preclinical studies and clinical trials have observed that THC alone or THC combination with CBD may be beneficial in the treatment of MS or symptom relief.2
Despite accumulating research supporting the potential of cannabinoids in the treatment of MS, more evidence is needed.3
The literature discussion is an overview of the published results from scientific studies investigating if and how cannabinoids can be beneficial in the treatment of Multiple Sclerosis. The overview will be updated regularly to ensure the newest and most accurate information.
CBD & PEA may express both anti-inflammatory and anti-demyelinating activities
In C57BL/6 mice, inflammation and neuronal demyelination were individually decreased by CBD and PEA .4
However, anti-inflammatory and anti-demyelinating activities were shown to be decreased by co-administration of both cannabinoids, proposing antagonism between both cannabinoid pathways.4
CBD and THC may be beneficial in the treatment of Multiple Sclerosis
In a mouse model of MS, Sativex oromucosal spray (50% THC and 50% CBD) was compared with each phytocannabinoid alone to assess their effect. It was observed that motor deterioration was similarly reduced by CBD-BDS and Sativex, whereas THC-BDS exhibited a weaker effect. The effect of CBD was via PPARγ receptors while THC effect was via CB2 and primarily CB1 receptors.5
In the rat model of experimental autoimmune encephalitis / multiple sclerosis, it was found that CBD exhibits immunoregulatory activities through induction of CD4+CD25−CD69+LAG3+ cells in MOG35-55-activated APC/TMOG co-cultures.6
Gene profiling found that CBD exhibits its immunoregulatory activities in activated memory TMOG cells via inhibiting pro-inflammatory genes, T cell proliferation, and potentially T-cell memory while enhancing anti-inflammatory genes.7
In the Experimental Autoimmune Encephalitis (EAE) mouse model of Multiple Sclerosis, it was shown that daily use of a 1% CBD cream could exhibit neuroprotective activities against EAE.8
Clinical trials are research studies that examine new treatments and evaluate their effects on human health outcomes.
THC and CBD appears to treat symptoms successfully – especially in patients not responding to conventional treatment
In several clinical trials, spasticity, muscle stiffness, neuropathic pain, etc. were treated by cannabis extracts or Sativex, a 50/50% mixture of synthetic THC and CBD in patients that did not show response to conventional treatment. 9,10
In an observational, prospective, multicenter, non-interventional study, symptomatic relief was achieved in 74.6% of patients upon treatment with THC/CBD mixture. 11
However, it was also reported that not all cannabinoids may produce a therapeutic effect on the symptoms of MS. 12,13
Treatment with THC may produce some side effects including dizziness and nausea. 14
One meta-study concluded that muscle spasms and central pain were reduced by several cannabinoids (particularly THC and CBD), whereas no effect was seen in treating tremors associated with MS. 15
- https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269
- https://ghmedical.com/endocannabinoid-system/diseases/multiple-sclerosis
- Zajicek, J.P., Apostu, V.I., (2011). “Role of Cannabinoids in Multiple Sclerosis”. https://link.springer.com/article/10.2165/11539000-000000000-00000
- Rahimi, A., Et Al., (2015). “Interaction between the protective effects of cannabidiol and palmitoylethanolamide in experimental model of multiple sclerosis in C57BL/6 mice”. https://pubmed.ncbi.nlm.nih.gov/25637488/
- Feliu, A., Et Al., (2015). “A Sativex(®) -like combination of phytocannabinoids as a disease-modifying therapy in a viral model of multiple sclerosis”. https://pubmed.ncbi.nlm.nih.gov/25857324/
- Kozela, E., Et Al., (2015). “Cannabidiol, a non-psychoactive cannabinoid, leads to EGR2-dependent anergy in activated encephalitogenic T cells”. https://pubmed.ncbi.nlm.nih.gov/25880134/
- Kozela, E., Et Al., (2016). “Pathways and gene networks mediating the regulatory effects of cannabidiol, a nonpsychoactive cannabinoid, in autoimmune T cells”. https://pubmed.ncbi.nlm.nih.gov/27256343/
- Giacoppo, S., Et Al., (2015). “A new formulation of cannabidiol in cream shows therapeutic effects in a mouse model of experimental autoimmune encephalomyelitis”. https://pubmed.ncbi.nlm.nih.gov/26489494/
- Rog, D.J., Et Al., (2007). “Oromucosal delta9-tetrahydrocannabinol/cannabidiol for neuropathic pain associated with multiple sclerosis: an uncontrolled, open-label, 2-year extension trial”. https://pubmed.ncbi.nlm.nih.gov/18035205/
- Zajicek, J.P., Et Al., (2012). ” Multiple sclerosis and extract of cannabis: results of the MUSEC trial”. https://pubmed.ncbi.nlm.nih.gov/22791906/
- Flachenecker, P., Et Al., (2014). “Nabiximols (THC/CBD oromucosal spray, Sativex®) in clinical practice–results of a multicenter, non-interventional study (MOVE 2) in patients with multiple sclerosis spasticity”. https://pubmed.ncbi.nlm.nih.gov/24525548/
- Ball, S., Et Al., (2015). “The Cannabinoid Use in Progressive Inflammatory brain Disease (CUPID) trial: a randomised double-blind placebo-controlled parallel-group multicentre trial and economic evaluation of cannabinoids to slow progression in multiple sclerosis”. https://pubmed.ncbi.nlm.nih.gov/25676540/
- Centonze, D., Et Al., (2009). “Lack of effect of cannabis-based treatment on clinical and laboratory measures in multiple sclerosis”. https://pubmed.ncbi.nlm.nih.gov/19768368/
- Wade, DT., Et Al., (2006). “Long-term use of a cannabis-based medicine in the treatment of spasticity and other symptoms in multiple sclerosis”. https://www.georgiacannabis.org/wp-content/uploads/2015/11/Wade-Sativex-MS-Spasticity.pdf
- Koppel, B.S., Et Al., (2014). ” Systematic review: Efficacy and safety of medical marijuana in selected neurologic disorders”. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4011465/
CANNABINOIDS & RECEPTORS
Below you find the plant cannabinoids, cannabinoid receptors, and endocannabinoids that are associated with the potential therapy.
If you have any further information relevant to the connection between Multiple Sclerosis and cannabinoids or find any of the information inaccurate, outdated or incomplete please contact us here.

